What is an AVM?
An arteriovenous malformation (AVM) is a malformation in the blood vessel system. There is a direct connection between an artery and a vein. read moreWhat is an AVM?
What is an AVM?
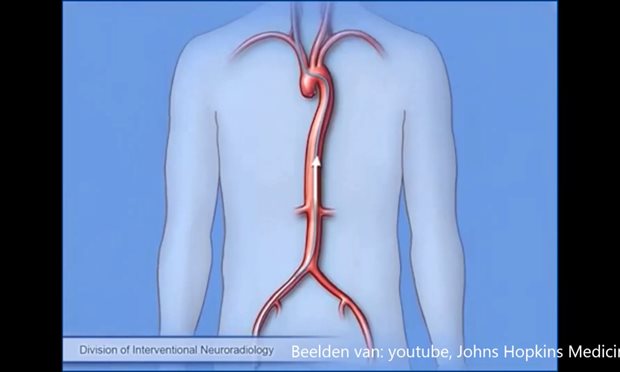
An arteriovenous malformation (AVM) is a malformation in the blood vessel system. There is a direct connection between an artery and a vein. Normally, a high-pressure artery feeds blood with oxygen. Via capillaries, it flows through to the brain cells. That is where the oxygen is released. The oxygen-depleted blood then enters the large efferent veins via small efferent vessels. These capillaries are missing in AVM. There is an abnormal tangle or network of vessels directly connecting the artery and the vein at that location. This causes high pressure on the efferent vein(s).Cause and formation
The cause of AVM in the brain is unknown. We think that a "predisposition" develops before birth, after which the AVM develops during life and is often expressed between 20th and 40th years of age.How often does an AVM occur?
An AVM is quite rare. It is unclear how many people have an AVM in the brain. Annually, 1 in 100,000 people are diagnosed with an AVM.Symptoms
Approximately 70% of all AVMs are detected without hemorrhage. This may be due to complaints in the form of an epileptic seizure, temporary speech disorders, or paralysis. We think this is due to a lack of oxygen supply to the relevant part of the brain. An AVM can also be discovered by accident, if for some other reason a scan of the head is made.Treatment
An AVM that has not hemorrhaged does not always require treatment. This is also undesirable in certain cases. Your attending physician will discuss this with you.If the AVM does require treatment, the aim of the treatment is to blocking the AVM completely in order to prevent hemorrhages or to reduce/stop complaints.
Tests and diagnosis
If you have an AVM, you will be referred to a neurosurgeon or neurologist specializing in cerebral blood vessels. In order to get a good picture of the AVM and how it communicates with the surrounding vessels, a vascular examination (angiography) is required. read moreTests and diagnosis
If you have an AVM, you will be referred to a neurosurgeon or neurologist specializing in cerebral blood vessels. In order to get a good picture of the AVM and how it communicates with the surrounding vessels, a vascular examination (angiography) is required.The treatment of the AVM requires an MRI of the brain in order to determine the location of the AVM and the surrounding brain tissue more precisely.
Life with an AVM
After a AVM, there are a number of things to consider. read moreAn AVM hemorrhage
The first symptom of an AVM is unfortunately often a brain hemorrhage, a form of stroke. read moreAn AVM hemorrhage
About the hemorrhage
Symptoms
Hospitalization after a hemorrhage due to AVM
Depending on your problems, you will be accompanied by physiotherapists, speech therapists, occupational therapists, and social workers.
In order to keep you and your loved ones informed of progress, weekly interviews will be organized with you, your medical team, and your loved ones during the hospitalization. During your admission after the hemorrhage, we will discuss a treatment plan with you and your loved ones.
Complaints
You may continue to have complaints that are both apparent and less apparent to others. Common examples of this are: (mental) fatigue, problems with processing stimuli, concentration problems, forgetfulness, and headaches. This can be quite a constraint on picking up your daily life again.
The nurse specialist will discuss follow-up appointments, advice on life rules, and taking up activities with you and your loved ones before being discharged.
Daily activities after an AVM hemorrhage
After an AVM hemorrhage, recovery from the hemorrhage is usually the first priority. AVM treatment usually follows at a later stage when your brain has recovered from the hemorrhage. Your attending physician will determine the correct timing of the treatment.
The effects of a brain hemorrhage on resuming your daily life vary widely, depending on the severity of the hemorrhage. You will receive advice on how best to resume your daily activities, work and hobbies from the nursing specialist, rehabilitation doctor, and/or company doctor.
If you are recovering from the hemorrhage, possibly while waiting for the AVM treatment, there is often uncertainty about activities that increase the pressure on the head. Examples include flying, diving, going on a roller coaster, pushing, going to the sauna, or having sex. There are no indications that these activities increase the risk of new AVM hemorrhage. These activities can therefore be carried out as usual.
Driving after an AVM hemorrhage
If you had an AVM hemorrhage, a driving suspension of 6 months after the hemorrhage applies. If, after this period, there are any residual symptoms that affect driving skills, a report from your specialist will be required. On the basis of this report, the CBR (Dutch Driving License Office) can decide whether an additional independent medical examination or a driving test will be required. Your medical specialist will write the report in addition to the CBR's declaration of health (website in Dutch).
Survivor stories Lammert
"It was a weird experience to hear how the ambulance came with for me "bells and whistles"." read moreSurvivor stories Lammert
Lammert is 50 years old, married, father of three children, and loves gardening. After his brain hemorrhage in 2014, he is now working as a police officer again.
1. When did you have a brain hemorrhage?
In November 2014 I had a brain hemorrhage as a result of an AVM. I was admitted to the Zwolle hospital for two weeks, of which I spent five days in intensive care. It was a weird experience to hear how the ambulance with came for me "bells and whistles". The same ambulance that I have had to call for many times at my own work.
2. How did your treatment go?
When I recovered from my brain hemorrhage, I was treated at another treatment center. The doctor glued the AVM closed via the groin. During the check-up it appeared that the AVM was not yet completely closed off, so I had to undergo surgery again. Since there was no certainty that this would be possible via the groin, I was now operated on via an incision in the bone. New technology made it possible to check whether the AVM had been completely removed during the operation. When I was still recovering on Intensive Care, the doctor came to tell me that the operation was 100% successful and that I would recover completely.
3. How do you look back on your recovery?
4. How did you experience the care?
The treatment and care made me and my family feel good. The attending physician gave a clear explanation about the disease and what had to be done. He also used the scans that were made. He always communicated openly, so we had a lot of confidence in the treatment. We also consider the support of the nursing specialist to be very positive. She is someone who is competent, knows what has been done, what still needs to be done, and is always available at short notice.
